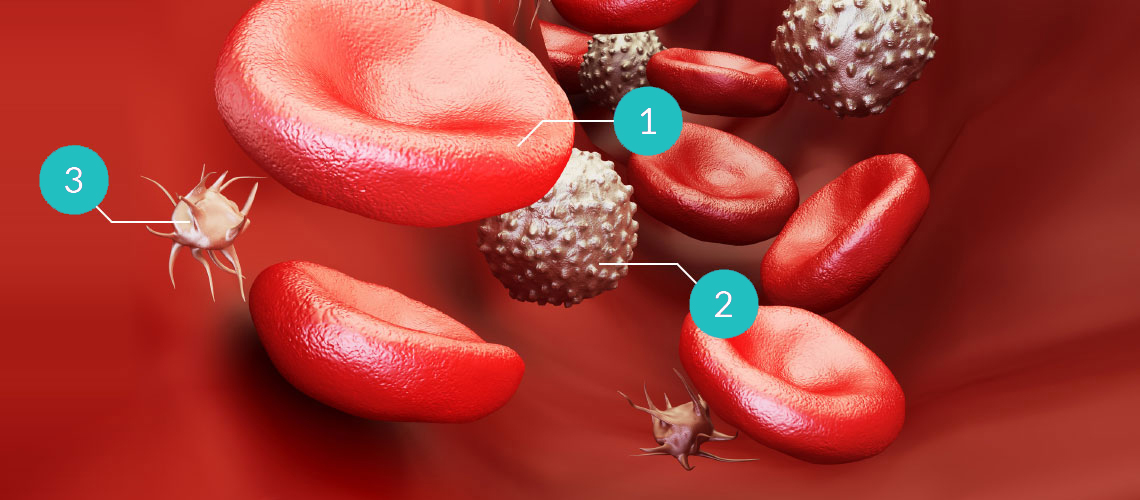
Platelets are responsible for hemostasis, and mediate the first phases of wound healing. In this phase, platelets aggregate and form the blood clot. In addition, growth factors are released by degranulation of thrombocytes.
The release of cellular growth factors supports healing by
- Attracting undifferentiated cells to the site of the injury (chemoattraction and migration) and by stimulating mitosis of undifferentiated cells (proliferation)
- Suppressing cytokine release, thus reducing anti-inflamma- tory reactions
- Attracting macrophages for the improvement of tissue healing and regeneration
- Supporting capillary growth and accelerating epithelization
Leukocytes form several cytokines, referred to as interleukins. They mediate between leukocytes and play an important role in immune defense.